The ADHD Brain: Investigating Distinct Wiring
Overview
With billions of neurons connected in complex networks that control our emotions, thoughts, and behaviors, the human brain is a marvel of intricacy. The brain circuitry of those who suffer from Attention Deficit Hyperactivity Disorder (ADHD) is different in minor but important ways. This article delves into the intriguing world of the ADHD brain, examining the distinct neural circuitry and how it plays a role in the disorder’s hallmark symptoms.
Comprehending ADHD from a Neurodevelopmental Angle
ADHD is a neurodevelopmental condition that interferes with day-to-day functioning and development due to persistent patterns of hyperactivity, impulsivity, and inattention. Although the precise etiology of ADHD is still unknown, research points to a potential interaction of neurological, environmental, and hereditary variables.
ADHD’s neurobiology
Studies on neuroimaging have shed important light on the anatomical and functional distinctions between the brains of neurotypical and ADHD sufferers. Among the important conclusions are:
Prefrontal Cortex Dysfunction:
People with ADHD show abnormalities in the prefrontal cortex, which is in charge of executive processes like working memory, impulse control, and attention. Difficulties maintaining focus and suppressing impulsive behaviors may be attributed to decreased activation and connectivity in this area.
Abnormalities of the Basal Ganglia:
The basal ganglia are important for motor control, reward processing, and the development of habits. The impulsive and hyperactive symptoms of ADHD are believed to be caused by a dysregulation of dopamine signaling in the basal ganglia.
Disparities in Connectivity:
Research on neuroimaging has shown that the brain areas responsible for motor control, sensory processing, and attention have different patterns of connectivity. These variations in brain structure could be a factor in the typical signs and symptoms of ADHD, like restlessness and distractibility.
The Function of Hormones
Chemical messengers called neurotransmitters let neurons in the brain communicate with one another. ADHD is linked to the dysregulation of specific neurotransmitter systems. Dopamine and norepinephrine are two neurotransmitters that are particularly noteworthy:
Dopamine:
Dopamine is essential for motivation, reward processing, and attention. Dopamine system dysfunctions are linked to deficiencies in motivational drive and reward sensitivity, which exacerbates feelings of boredom and inattention in ADHD sufferers.
Norepinephrine:
This hormone is important in attention management, alertness, and arousal. Norepinephrine signaling dysregulation is assumed to play a role in the challenges faced by ADHD sufferers in sustaining attentiveness and attention.
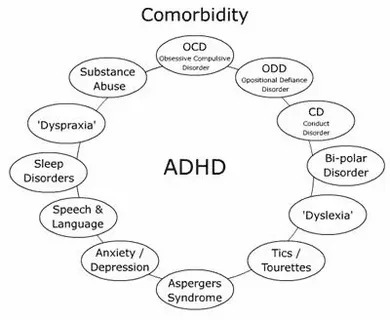
ADHD Heterogeneity
It’s critical to understand that ADHD is an illness that affects people differently. The presentation of ADHD varies greatly throughout people, with subtypes ranging from primarily inattentive to primarily hyperactive-impulsive. Variabilities in underlying brain systems and genetic predispositions could be the cause of this variability.
Treatment Consequences
Treatment and intervention options will be significantly impacted by our growing understanding of the neuroscience of ADHD. While behavioral therapy and medication are frequently used to manage the symptoms of ADHD, new research points to the possibility of more focused interventions that target particular neurobiological deficiencies. These could consist of:
Stimulant drugs:
The most often prescribed therapies for ADHD are stimulant drugs like amphetamines and methylphenidate. They function by making more dopamine and norepinephrine available in the brain, which enhances focus, impulse control, and hyperactivity.
Non-Stimulant Medications:
These drugs, which target distinct neurotransmitter systems, include atomoxetine and guanfacine. They can be used as substitutes for stimulants in patients who don’t respond well to them or who have unpleasant side effects.
Cognitive Training:
Programs aimed at enhancing executive functioning—such as working memory, cognitive flexibility, and inhibitory control—have the potential to alleviate symptoms associated with ADHD. The brain pathways underlying impulse control and attention may be strengthened by these programs.
Neurofeedback is the process of monitoring brain activity in real time by functional magnetic resonance imaging (fMRI) or electroencephalography (EEG), and then giving the person feedback to assist them learn how to control their brain activity. Neurofeedback is still regarded as experimental, although it may be a non-invasive ADHD intervention.
In summary
The distinctive patterns of neural connection and neurotransmitter dysregulation found in the ADHD brain contribute to the disorder’s characteristic symptoms. Researchers and clinicians can better target and effectively treat individuals with ADHD by developing a greater knowledge of the neurobiology of the disorder. We are making progress in deciphering the workings of the ADHD brain by persistent study and creative thinking, which opens doors to new understandings and treatments for individuals impacted by this intricate disorder.